5-alpha-reductase deficiency (5 ARD)
5-alpha reductase type 2 deficiency (5 ARD) is a genetic anatomical difference. 5 ARD enzymatic disturbances result in the body’s inability to convert testosterone into dihydrotestosterone (DHT).
DHT is required for typical external male genitals to develop, so genetic males (with XY chromosomes) with 5 ARD are born with variations in genitals.
That means when these babies are born, it can be hard to tell without further testing if they are male or female. It can also mean genitals and reproductive organs are likely to vary.
People with 5 ARD may be brought up as girls or boys, though more frequently, this choice is left up to the child – who are generally very clear about their views.
It can be important, however, for some decisions to be made on behalf of the child, since surgical and hormonal interventions can play a large role in future body satisfaction.
5 ARD only affects boys in any significant way, since girls with this condition have few consequences, and retain typical fertility and genitalia. A female may never know she has this genetic variation.
Boys, on the other hand, usually have greater challenges. 5 ARD people are genetic males who missed out on some critical male genital development, which defaults to female in the absence of certain hormonal triggers. The degree of difference in genitalia and reproductive organs varies considerably.
Classic presentation of 5 ARD
There may be a clitoris-like phallus, a cleft in the midline of the scrotum caused by incomplete fusion (a bifid scrotum), half-female half-male-looking genitalia (pseudovaginal perineoscrotal hypospadias, PPSH), and what appears to be a version of a prostate.
People with 5 ARD may appear more masculine in the genital area, without a separate vaginal opening, and a blind vaginal pouch that opens into the urethra, and perhaps the atypical positioning of the very end of the urethra on the penis (penile hypospadias). Those with 5 ARD are without a uterus or fallopian tubes due to typical secretions from the intact testes (which don’t rely on androgens for development) of Müllerian-inhibiting factor.
Those with 5 ARD have seminal vesicles, vasa deferentia, epididymides, and ejaculatory ducts, with a small prostate that can’t be felt, and isn’t thought to cause prostate problems (cancer, benign prostatic hyperplasia).
Causes of 5 ARD
5-ARD is caused by an enzyme deficiency that leaves the body with high testosterone, but low DHT, which is the more bioavailable form of androgen.
Two genes have been identified, with many, many mutations. 5-ARD occurs more frequently in the Dominican Republic, some New Guinea tribes, and in Turkey. There are more than 50 families with this condition in several places around the world. Some have no genetic mutations so far found.
What 5-ARD looks like in real life
The Prader Scale shows the degree of virilisation
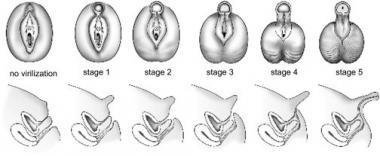
The external genitalia look like labia, with some rugation (folds, waves) and sometimes pigmentation. The phallus can be from 1cm (like a clitoris) to 2cm, which is the lower limit for a typical penis.
The testes are usually in the inguinal canals on either side of the groin, but can be found in the labioscrotal folds or even in the abdomen.
The vagina usually ends in a blind pouch (vaginal hypoplasia), but a hymen is usually present and appears typical. The uterus is absent (müllerian aplasia).
When puberty hits, what do we see?
Boys (46 XY DSD)
Clear signs of a boy turning into a man appear – narrow hips, broad shoulders, penis enlargement, Adam’s apple may appear, the voice deepens, and facial hair may develop. Muscles may thicken, and body hair can increase.
Breasts do not develop most of the time, and the vaginal entrance remains atrophic (staying red, not pink – vaginal mucosa turns pink with oestrogen).
Girls (46 XX)
Females have more subtle impacts – delayed menstruation, very little or no acne, very light body hair. Fertility remains typical in 46 XX females.
Diagnosis of 5-ARD
This genetic disposition is discovered at birth by identifying variations in the appearance of genitals. This can be misdiagnosed as complete androgen insensitivity syndrome (CAIS), which looks practically identical.
Diagnosis may take some time in those with enlarged clitorises (clitoromegaly) or external genitalia that appears typical. These cases will be discovered at puberty, when menstruation fails to appear, with some other symptoms including a lack of more grown-up male characteristics appearing.
Tests will include karyotype with specific X and Y probes (a genetic test), tests for 17-hydroxyprogesterone, follicle-stimulating hormone (FSH), luteinising hormone (LH), testosterone, dihydrotestosterone (DHT), anti-mullerian hormone (AMH), electrolytes, urinalysis, and an ultrasound to assess for the presence of internal male or female structures.
There is some evidence that 5-ARD in elite female athletes with hyperandrogenemia may be 200 times that of the general population. A child with variations in genitalia will have a special team assess their case.
Treatment and management of 5-ARD
There is no treatment as such for 5-ARD, but management strategies for adverse symptoms and gender assignment and identification.
Delaying any irreversible surgical procedures has recently developed after individuals expressed their dissatisfaction with decisions that were made without their consent. There is nothing known that a pregnant woman or father can do to prevent this.
Caring for 46 XY DSD people
Frank, open discussion is required regarding gender identity, gender assignment, gender roles, and sexual satisfaction. These subjects have undergone significant upgrades in terms of conversations in the past two decades, and so has the care provided, for the better.
Surgery should not be rushed, nor should an attempt to force a gender onto the child. Informed consent means a lot to these kids who then become adults – making decisions on their behalf that will impact the rest of their lives needs to be done with great care and consideration.
Understanding that a child with 5-ARD is unlikely to be fertile, may struggle with sexual satisfaction, and genital satisfaction is important, and each situation will be different based on the presentation of the child’s genitals.
Hormone replacement therapy in 5-ARD
Hormone replacement therapy will be dictated by surgical outcomes.
- For those raised as males, DHT therapy may increase penis length, given both as children and at puberty. Males with intact gonads do not suffer bone mineral density losses.
- For those raised as females, oestrogen replacement therapy should be initiated at age 12 or at increased gonadotropins (if earlier). Progesterone therapy is not usually required (due to no uterus). Females can suffer bone mineral density losses – adjust as necessary.
Genital surgery in 5-ARD
Some feminising surgical interventions include:
- Gonadectomy (removal of the testes, laparoscopic)
- Labioscrotal fold restructures into labia
- Reduction/recession of phallus to give the appearance of a clitoris (with function)
- Clitoroplasty (keeping clitoral glans and sensory input)
- Separation of the urethra from the vagina
- Vaginoplasty
- Colovaginoplasty
There are those who chose the female identity for those with 5-ARD, which must occur before the child is exposed to too much androgen, which allows for a more stable female gender identity, and avoids the pubertal problems, including surgery.
Others recommend waiting until the child is past puberty, when they can decide for themselves if they want reconstructive surgery, and can better care for themselves afterwards with dilators.
Once a gonadectomy is performed, fertility options disappear no matter what the person decides. Pregnancy and childbirth are impossible due to a lack of uterus and possibly other structures.
Surgery for male gender assignment includes:
- Urethroplasty (urethral surgery)
- Repair of bifid scrotum (a crease in the middle of the scrotum)
- Chordee repair (a downward-facing penis with the urethra on one side)
- Orchiopexy (repair of undescended testes)
DHT therapy helps males, but many forms are not available in all countries. Giving testosterone to children has implications for the skeleton, but after puberty, can help with a sense of wellbeing and physical changes to their male advantage. A small penis presents its own problems since current techniques are either short-acting or ineffective. Males may be fertile, but IVF is required, with sperm counts low, abnormal spermatogenesis, and thick ejaculate.
Surgical complications in 5-ARD
Urinary tract problems, decreased clitoral sensation, and vaginal or vaginal entrance narrowing are risks. Male identified can end up with urethral fistulas and closing of the urethral tube.
Psychological complications
A psychologist experienced in this condition should be employed from the beginning for both the 5-ARD individual and their parents.
References
- Arboleda VA, Sandberg DE, Vilain E. DSDs: genetics, underlying pathologies and psychosexual differentiation.Nat Rev Endocrinol. 2014;Oct;10(10):603-15. doi: 10.1038/nrendo.2014.130. Epub 2014 Aug 5.
- Vilain E. The genetics of ovotesticular disorders of sex development. Adv Exp Med Biol. 2011;707:105-6. doi: 10.1007/978-1-4419-8002-1_22.Wiersma R. The clinical spectrum and treatment of ovotesticular disorder of sexual development. Adv Exp Med Biol. 2011;707:101-3.
- Hughes IA, Houk C, Ahmed SF, Lee PA; Lawson Wilkins Pediatric Endocrine Society/European Society for Paediatric Endocrinology Consensus Group. Consensus statement on management of intersex disorders. J Pediatr Urol. 2006;2(3):148-62.
- Kim KR, Kwon Y, Joung JY, Kim KS, Ayla AG and Ro JY. True hermaphroditism and mixed gonadal dysgenesis in young children: A clinicopathologic study of 10 cases. Modern Pathology. 2002;15(10):1013-1.
- Hutcheson J, Snyder III HM. Ambiguous Genitalia and Intersexuality. Medscape.
- Medline Plus: A Service of the U.S. National Library of Medicine and the National Institutes of Health. Medical encyclopedia: Intersex.
- Ahmed F, Lucas-Herald A, McGowan R, Tobias E. Orphanet.
- NORD Rare Diseases, Eric Vilain, MD, PhD, Professor of Human Genetics, Pediatrics and Urology; Director, Center for Gender-Based Biology; Chief, Medical Genetics, Department of Pediatrics; David Geffen School of Medicine at UCLA





