Understanding and treating aerobic vaginitis (AV)
Aerobic vaginitis (AV) is an inflammatory vaginal microbial condition. Aerobic means the bacteria that dominate the vaginal flora prefer to live in an environment with oxygen, while vaginitis means vaginal inflammation.
Many AV-related bacteria can survive in anaerobic (oxygen-free) conditions and are known as facultative anaerobes.
AV can cause some very uncomfortable symptoms, and comes with complications such as preterm labour, increased risk of contracting sexually transmitted infections, and abnormal Pap test results. AV may on the surface be frequently confused with bacterial vaginosis (BV).
Diagnosis of aerobic vaginitis
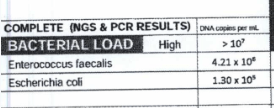
Diagnosing aerobic vaginitis requires a positive test with the dominant strain in the vaginal microbiome being one or more of the AV-causing bacteria, alongside a loss of healthy lactobacillus species, and sometimes an elevated vaginal pH reading. A doctor will also look for certain vaginal indicators.
The most useful test for the bacterial profile of your vagina is a comprehensive microbiome panel (we love Juno Bio), which can be ordered by your practitioner or bought online yourself and done at home.
These incredible vaginal microbiome tests offer a full picture of the types and amounts of bacteria and fungus/yeast living in your vagina, microbial load, and a pH snapshot.
Most common aerobic vaginitis bacteria
- Escherichia coli
- Enterococcus faecalis
- Group B Strep Streptococcus agalactiae
- Staphylococcus aureus
- Staphylococcus epidermidis
- Klebsiella
Symptoms of aerobic vaginitis
- Inflammation of the vagina and/or vulva
- Redness
- Itching
- Soreness
- Possibly ulcers or erosions
- Changed vaginal odour
- Rotten, foul odour
- Burning
- Stinging
- Swelling
- Painful sex (dyspareunia)
- Yellowish/greenish discharge
- Thick, sticky or irritating discharge
- pH of 4.5 or more (test vaginal pH at home)
- Signs of atrophy on vaginal cells
- Possibly long-lasting symptoms after multiple unsuccessful treatments
Understanding treatment for aerobic vaginitis
The typical treatment for AV is antibiotics, which can work very well for straightforward cases of local vaginal infection. But, AV can point to a greater systemic microbiome problem (gut, urinary tract, pathways) that may benefit from broader investigations and non-drug treatments.
AV can be tricky, so it is My Vagina’s recommendation that you book with one of our vulvovaginal specialist naturopathic practitioners for individualised care and practitioner only treatments.
You can find information and treatment recommendations for AV in Killing BV, My Vagina’s exceptional vaginal dysbiosis guide.
Killing BV includes a greater discussion of bacterial biofilms and why BV and AV can evade antibiotics, and provides a treatment guideline using our effective AV blend vaginally.
The addition of Aunt Vadge’s Oral UTI Herbal Blend is also recommended, as even if you don’t have urinary tract symptoms, the blend is designed for AV bacteria (which are also UTI bacteria) and will treat your whole system.
A rinse with povidone-iodine (also known as iodopovidone) may provide short-term relief of symptoms, but bacteria will likely return.
Don’t continue any treatments if your symptoms worsen. Seek qualified, experienced specialist support.
Antibiotic treatment of aerobic vaginitis
Local antibiotics may be prescribed, often broad-spectrum to cover gram-positive and gram-negative aerobes (like kanamycin). Oral treatments with amoxiclav or moxifloxacin may be used, particularly if group B strep or methicillin-resistant Staphylococcus aureus (MRSA) is present.
Oral antibiotic use is discouraged in those with aerobic vaginitis, with topical treatments favoured by doctors due to low absorbency and high concentrations where it matters.
Treatments should maximise the survival of lactobacilli species where possible, while effectively killing gram-negative bacteria like E. coli, S. aureus and E. faecalis. Combination treatment may be most appropriate due to antibiotic resistance, but your doctor will prescribe based on your circumstances and the latest drug recommendations
Knowing the specific bacteria in your vagina via a comprehensive vaginal microbiome test is useful for targeted treatment. Discuss a microbiome panel with antibiotic sensitivities/resistance genes with your doctor.
The most common causes of AV are E. coli and E. faecalis. It’s possible to have vaginal flora in AV that also includes protective lactobacilli, just fewer.
Antibiotic vaginal gel and hydrocortisone suppositories may be effective in eradicating aerobic vaginitis.
Some antibiotics are problematic and won’t work, and resistance is common in some countries. Talk to your doctor about their recommendations.
The relationship between AV and UTIs
AV-related bacteria are implicated in urinary tract infections (UTIs), and the bacteria can migrate back and forth between the vagina and urinary tract due to close proximity.
In the case of frequent/chronic UTI, just treating the vagina is unlikely to yield long-lasting results, but symptom management as the UTI issue is resolved via other means can be achieved.
A culture is usually the first step a doctor will take to diagnose AV, but a full vaginal microbiome panel offers the best picture of all bacteria and yeast in the vagina, unlike a culture, which will only find dominant, culturable species.
Cultures are a reasonable first step, but do not provide a breakdown of all bacteria and fungus in the sample. A full microbiome report offers a comprehensive picture and is the standard My Vagina practitioners use and recommend.
Most medical doctors, however, do not yet use these tests as the norm and may not know how to interpret them. In that case, your practitioner can book in for a quick Practitioner Microbiome Analysis with one of our vaginal microbiome specialists – refer them to My Vagina Pro, our practitioner portal.
AV may be assumed to be BV or yeast, depending on presenting symptoms and therefore may not be diagnosed or treated appropriately at first. If your doctor does a culture and says they can’t find anything wrong, get yourself a comprehensive microbiome test and find a practitioner who can help.
The relationship between AV and CV
There is a specific situation where flora switches between AV and cytolytic vaginosis (CV). The microbiome goes from being dominated by aerobic vaginitis-associated bacteria such as Escherichia coli and Enterococcus faecalis to a very high proportion of usually Lactobacillus crispatus, from 98 per cent and upwards of just the one lactobacilli species.
It’s important to note that if, for example, there was 98 per cent of L. iners, at My Vagina, we would not consider this CV (read more about L. iners dominant flora). It is very specifically L. crispatus in this AV-CV scenario, possibly L. gasseri or L. jensensii, but they are much less common.
Dominance of L. crispatus by itself is not a diagnosis of CV, and may be healthy for that person in the absence of symptoms. CV’s main symptom of burning, and may include irritation, itching and thick or stringy white discharge.
Determining CV relies on the presence of symptoms, and a high amount on a test result is not definitive. Do not self-diagnose CV! It is a very specific condition and you need help to work out what’s going on.
The presentation of AV and then CV (and vice versa) is a symptom picture that gives us a lot of clues. The vaginal cells are offering safe harbour only to certain types of bacteria (L. crispatus, E. coli, E. faecalis), and that’s why they can switch back and forth in this very specific way.
You might treat AV bacteria, but another just takes its place in a never-ending merry-go-round, possibly switching from AV to CV and back again. This switching indicates you have an underlying contributing cause and need to consider your symptoms are not a bacteria or underneath, not even a vagina problem, but something else.
It is this underlying problem, not just the vaginal microbiome, that must be corrected or treatment will continue to fail.
If it’s not one problem bacteria, it’ll be another, because the cells are not able to hang on to their healthy lactobacilli species. Once the underlying issue is solved, the vaginal cells will return to normal and healthy change can occur and be maintained.
When AV turns into DIV
The most severe form of aerobic vaginitis is called desquamative inflammatory vaginitis (DIV) but DIV may not be associated with bacteria.
We recommend whenever you have vaginal symptoms or a suspected infection to get a comprehensive microbiome test for the full picture.
Understanding the gut microbiome in AV and chronic UTI
The reason for this possible treatment complexity is aerobic bacteria and pathogens may be commensal (normal, healthy) in other areas of the body such as the digestive tract, but have colonised the vagina or urinary tract, causing symptoms.
There may be to be a larger body-wide bacterial imbalance occurring, so treating the vagina alone may be missing the true problem.
If, for example, you have an abundance of E. coli and E. faecalis in the digestive tract, it isn’t a huge stretch to see how that abundance, in the right conditions, could spill over into the vagina and urinary tract – there is only so much real estate for bacteria on your cells, so more of one sort means less of other, more protective species. You may not have digestive symptoms, but this doesn’t mean you do not have an imbalance.
Getting the right help
We’re in complex territory here, and there’s no reason you should know what to do or what is wrong. We have practitioners for this, who care about germs and symptoms and spend their spare time getting delighted over diseases so that you don’t have to.
A good first step is to download Killing BV, as a lot of the information applies to AV as well as BV, and it’ll provide a good understanding of the vaginal ecosystem.
Book with a My Vagina vulvovaginal specialist naturopath or another practitioner who deeply understands the vaginal microbiome and its relationship to the rest of dthe body.
Drug treatments include antibiotics for the bacterial component, steroids for inflammation, and possibly oestrogen therapy depending on which doctor you see.
Non-drug approaches may include vaginal treatments (Aunt Vadge’s AV pessary blend), but further investigations may be in order, such as diagnostic testing.
Working on both the symptoms and underlying causes in the individual is important when AV is chronic. Contributing causes might be hormonal, immunological or genetic, but each person is assessed and treated individually.
References1–5
- 1.Donders GGG, Bellen G, Grinceviciene S, Ruban K, Vieira-Baptista P. Aerobic vaginitis: no longer a stranger. Research in Microbiology. Published online November 2017:845-858. doi:10.1016/j.resmic.2017.04.004
- 2.Casa V, Noll H, Gonser S, Grob P, Graf F, Pohlig G. Antimicrobial Activity of Dequalinium Chloride against Leading Germs of Vaginal Infections. Arzneimittelforschung. Published online December 26, 2011:699-705. doi:10.1055/s-0031-1299954
- 3.Jahic M, Mulavdic M, Nurkic J, Jahic E, Nurkic M. Clinical Characteristics of Aerobic Vaginitis and Its Association to Vaginal Candidiasis, Trichomonas Vaginitis and Bacterial Vaginosis. Med Arh. Published online 2013:428. doi:10.5455/medarh.2013.67.428-430
- 4.Donders GGG, Ruban K, Bellen G. Selecting Anti-Microbial Treatment of Aerobic Vaginitis. Curr Infect Dis Rep. Published online April 22, 2015. doi:10.1007/s11908-015-0477-6
- 5.Mendling W, Weissenbacher ER, Gerber S, Prasauskas V, Grob P. Use of locally delivered dequalinium chloride in the treatment of vaginal infections: a review. Arch Gynecol Obstet. Published online October 27, 2015:469-484. doi:10.1007/s00404-015-3914-8





