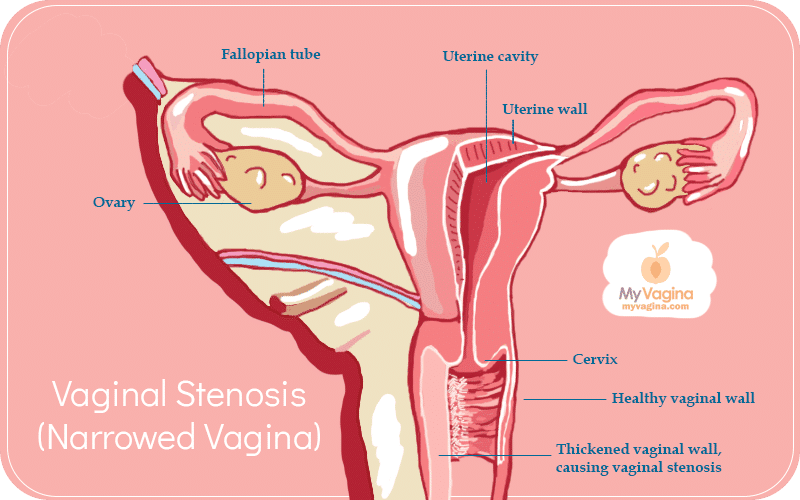
Radiation-induced vaginal stenosis (narrowing of the vagina)
Vaginal stenosis is the medical name for narrowing of the vagina, often with a loss of elasticity.
Stenosis most often occurs as a negative outcome of external beam radiotherapy, brachytherapy, and/or vaginal/pelvic surgery. Typically vaginal stenosis comes with vaginal dryness and poorly-functioning scar tissue.
Read more about pelvic radiation and its effect on your vagina here.
The extent of vaginal stenosis depends on where the cancer is, the treatment type and dose, scheduling of doses, any concurrent chemotherapy, the patient’s age and sensitivity to the radiation.
There isn’t a lot of research into post-radiation vaginal stenosis, but a growing pool of post-treatment cases exists. A review looked at rates of reported vaginal stenosis, putting the number at between 1.25 per cent to 88 per cent.
Radiation-induced vaginal stenosis is understood to be a common, underreported side-effect of pelvic radiation that usually occurs within the first year after radiation and gets worse over time.
Incidence of radiotherapy-induced vaginal stenosis
One study of 54 patients reported that vaginal stenosis increases over time, with the first year after follow-up usually about a grade one, with moderate-to-severe stenosis increasing up to three years post-treatment.
Another study of women with stage 1B to stage IV cervical cancer treated with radiotherapy or a combination of radiotherapy and brachytherapy recorded the incidence of vaginal stenosis at 38 per cent.
What vaginal stenosis feels like
The most common cause of vaginal narrowing and tissue damage is radiation therapy for cancer of the vagina, bladder, lymph glands, uterus, cervix or rectum.
The radiation may be applied externally or internally, but always has a negative impact on vaginal tissue, causing thinning, drying, scar tissue formation, and a shortening and narrowing of the vaginal canal.
Blood vessels are reduced in number, making the tissue fragile. Low blood flow results in poor vaginal tissue performance and can make sex very uncomfortable or painful. Sex may cause bleeding.
The vulva may suffer, shrinking and atrophying, and be easily torn from wiping after the toilet. The cancer may have caused premature menopause, with a lack of oestrogen perpetuating the problem, since vulvar and vaginal tissue is very sensitive to oestrogen.
Oestrogen has a protective and stimulating effect on vulvar and vaginal cells.
What happens to vaginal tissue in vaginal stenosis
The vaginal lining (mucosa) covers muscle fibres. Vaginal stenosis is caused when the mucosa becomes inflamed, blood vessels proliferate (hyperaemia), and the top layer of cells degrade and disappear (denudation), resulting in ulcers and tissue injury.
This denudation results in blood vessel issues like small-vessel thrombosis, swelling and the degradation of muscle. The vaginal mucosa is damaged by increased collagen production in the submucosal connective tissue layer, leading to changes in the vaginal mucosa.
Tissue changes can lead to the muscles and blood vessels being obliterated, resulting in a lack of oxygen to tissue, and tissue scarring and thickening.
Risk factors for vaginal stenosis
- Those over 50 years of age
- Cigarette smoking
- Assessment of grade II vaginal pallor reaction at six months
Treating vaginal stenosis – the sooner you start, the better
There are several methods used to keep the vagina functional, including the use of vaginal dilators to stretch the tissue out over time. These dilators require regular use, from the very beginning, to be effective.
The sooner you start using them, the better the outcomes over time. Talk to your specialist about recommendations for your case.
Oestrogen creams containing just E3 (oestriol) may also be useful, along with pelvic exercises.
Additionally, a study looked into a combination of olive oil, pelvic floor exercises, and a vaginal moisturiser and found this to be an effective and cheap way to improve vaginal function.
Read more about the OVERcome study here.
Navigating sex and relationships with a narrowed vagina
Depending on your treatment, sex and contraception use may be out of the question at least temporarily, but your specialist will talk this over with you.
There are also a handful of excellent support groups where women have come before you, with the same problems. You can share your story, get tips on how to manage your vagina, and see what other people’s specialists are saying.
Having cancer of any kind is scary, but when the effects of cancer treatment affect such an intimate part of you, it can be even harder to talk about. Your narrowing vagina is not really dinner party conversation in most circles, and even confiding in a close friend can feel embarrassing. This means we often keep these horrible side-effects secret.
If you have a partner, having an out of commission vagina can make intimacy impossible or very difficult and painful. Navigating your relationship with these changes can be challenging to say the least, so getting good advice and support from your specialists and support groups is important.
Figuring out how to have hard conversations about sex is not something most of us are very good at, but finding your words and understanding your limitations is a necessary element.
Don’t underestimate the impacts of your cancer treatments on your vagina, and put strategies in place early on.
How natural medicine can help support you post-cancer
There are many practitioners that can support you on your post-cancer journey, from acupuncture, massage, reflexology and other manual therapies, to sex therapists that specialise in treating people and couples in your position.
There may be herbal creams or medicine that can boost normal tissue repair, and diet modifications to ensure your body is getting everything you need to repair.
References
Morris L, Do V, Chard J, Brand AH. Radiation-induced vaginal stenosis: current perspectives. International Journal of Women’s Health. 2017;9:273-279. doi:10.2147/IJWH.S106796.