-
×
 Killing BV System: Vagina Treatment Guide and Membership
1 × USD $0.00
Killing BV System: Vagina Treatment Guide and Membership
1 × USD $0.00
Clitoridectomy
There are several reasons why a clitoris may be removed in an operation called a clitoridectomy.
These causes include clitoral hypertrophy1 (an oversized clitoris possibly caused by congenital adrenal hyperplasia (CAH), drugs or other interference), female genital mutilation, or possibly another disease or accident.
Surgery to remove part or all of the clitoris – the clitoridectomy
The decision to remove part of the clitoris is not one taken lightly by surgeons, the owner of the clitoris, or her caregivers if the clitoris belongs to a young girl.
The ability to orgasm shouldn’t be impeded for the sake of looking ‘normal’2, but sometimes the circumstances favour losing the appendage.
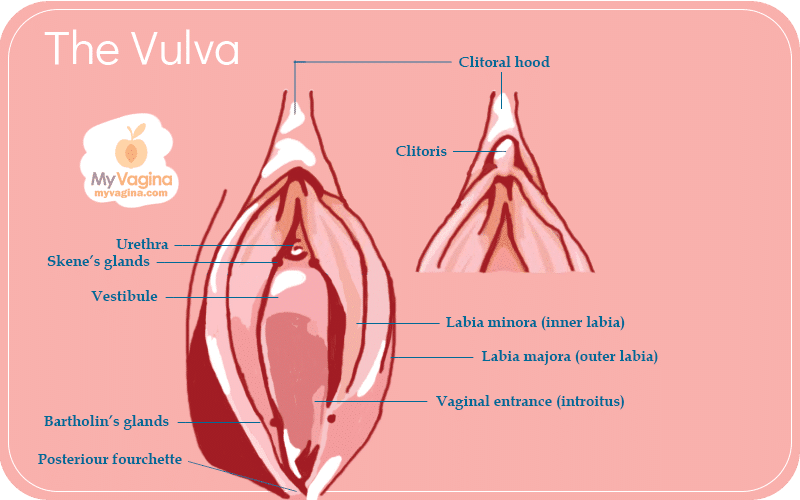
A normal clitoris and clitoral hood
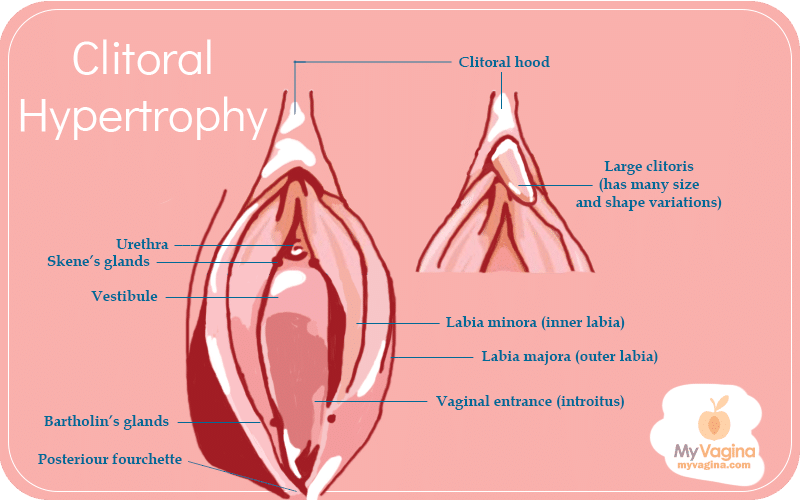
Clitoral hypertrophy
Outcomes of clitoridectomy surgery
Loss of sensation and neurological damage cannot be ruled out after a clitoridectomy3, as the clitoris is a very delicate part of anatomy4. After surgery, the external and visible part of the clitoris may be missing partially or fully.
In most people undergoing clitoridectomy, orgasm can still be achieved. This is very carefully evaluated on a case-by-case basis.
The focus of a clitoridectomy is for the patient to have a normal life, including a normal sex life. This means the vagina and vulva look and behave like normal, without pain in sexual activity.
The clitoridectomy operation has been revised several times over the years; however, loss of sensation is a very real risk. Burying the glans is also problematic since the trapped tissue causes pain when stimulated (engorged); however, with the removal of the clitoris (or at least 50 per cent of it), full sensation and function have been observed. The younger one is when this operation is undertaken, the better the outcomes.
With a macroclitoris (an enlarged clitoris), the operation is relatively simple to remove excess tissue, but complications can include excessive bleeding from the veins at the base of the clitoris and nerve damage.
The surgeon is responsible for ensuring the blood supply and nerves remain intact and that, if ruptured, bleeding is controlled. Nerve damage can be a little harder to predict, so a very experienced surgeon should be sought.
The clitoridectomy surgery
- An example of a 5 cm hypertrophied clitoris – the end of the clitoris is clamped to hold it steady, and a scalpel is used to cut the end of the clitoris off. The cut is wedge-shaped, so there is a small V. This allows the labia to be stitched up to cover the gap.
- Cutting the clitoris off is a delicate procedure that involves very careful manipulation of the blood supply to avoid extensive bleeding.
- Once stitched up, the vagina looks relatively normal. A lot of clitoral tissue (which is extensive beyond what we can actually see and directly touch) still remains.
Other treatments that may be included with a clitoridectomy
Hormone therapy (HT) and surgical reduction are indicated when hormonal problems have been identified as the cause of an abnormal clitoris. The surgery may be for psychological and aesthetic reasons, which means it is not functionally necessary and may be considered avoidable in some cases.
The goal of any treatment is to offer the greatest chance of retaining sensitivity and caring for the person’s emotional needs.
Techniques for clitoridectomy
There are several documented methods to remove part or all of the clitoris
- Amputation (the complete removal) of the clitoris
- Bending the clitoris over and attaching it to the pubic bone
- Removing part of the corpora cavernosa
- Severing the clitoris at the root, then reattaching the glans as a graft
- Shortening and cutting off the corpora cavernosa
The key features of the surgery are preserving the neurovascular pedicle (a stalk-like structure) and maintaining the sensitivity of the glans clitoris.
Sex after a clitoridectomy
Every clitoris has its own story to tell, with the technique used in the surgery – including female genital mutilation techniques – largely determining what happens with sexual pleasure, arousal and orgasm. Whether you are on your own or with a partner, the scar tissue and rearrangement of tissues will be unique to you.
Also unique is what turns you on and what areas of your body are sensitive. While it seems incredible, some people (lucky things!) can orgasm from nipple stimulation alone, but this is not the norm. This means that most of us require a set of psychological cues plus physical stimulation to be aroused and reach orgasm.
It’s important to note that the clitoris has larger structures, legs and arms and is actually quite a big structure inside the pelvis compared with the outer portion (glans). The inside of the vagina provides access to the structures of the clitoris, which become erect upon arousal, like penile erectile tissue.
If you have never had an orgasm, and your clitoris has been cut, there isn’t anything to compare it to. This means you’re on your own in figuring out what you like and don’t. Most people can find sexual pleasure and orgasm since, luckily, regular physiology means that’s possible.
Having part of a clitoris or no clitoris does not mean no orgasm. It can mean no orgasm for a small percentage of people, depending on the damage, and a bit or a lot more work for many of you. Some of you, however, will have absolutely no issue with orgasm after a clitoridectomy.
An experienced sex therapist experienced in this field can guide you on how to find sexual satisfaction if you are finding it challenging. Find support groups, talk to others who are in the same position, and find strategies that work for you.
References
- 1.Randolph JG, Hung W. Reduction clitoroplasty in females with hypertrophied clitoris. Journal of Pediatric Surgery. Published online April 1970:224-231. doi:10.1016/0022-3468(70)90279-4
- 2.Kirby V. On the cutting edge: Feminism and clitoridectomy. Australian Feminist Studies. Published online December 1987:35-55. doi:10.1080/08164649.1987.9961564
- 3.Kandela P. Clitoridectomy. The Lancet. Published online April 1999:1453. doi:10.1016/s0140-6736(05)75985-7
- 4.Longhurst GJ, Beni R, Jeong SR, et al. Beyond the tip of the iceberg: A meta‐analysis of the anatomy of the clitoris. Clinical Anatomy. Published online September 29, 2023:233-252. doi:10.1002/ca.24113
USD $0.00 ex GST/VAT/TAX
REVAMPED!
USD $0.00 ex GST/VAT/TAX





